INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is considered the “gold standard” treatment for degenerative cervical disease with instability and kyphosis involving two or more levels [1,2]. With the development of various surgical materials, such as synthetic cages and bone-inductive substances, cervical stability and fusion rates after ACDF have significantly improved [3-7]. The i-Factor bone graft (Cerapedics Inc, Westminster, Colorado) (i-factor), a bone substitute material, is a combination product consisting of P-15, which is adsorbed onto anorganic bone mineral suspended in an insert biocompatible hydrogel carrier. Evidence of the bone-forming ability of i-factor has been demonstrated in pre-clinical models and clinical investigations [8-10]. Recently, several studies have revealed that ACDF with i-factor demonstrated a superior fusion rate compared with local autograft bone [11,12]. However, there is no guideline on the exact number of doses of i-factor per level that should be used when performing ACDF, and there has been no study on the adverse effects of i-factor.
Herein we discuss two cases that presented unexpected bone formation after ACDF using polyetheretherketone (PEEK) cage with i-factor.
CASE REPORT
Informed consent was obtained from all individual participants included in this study.
1. Case 1
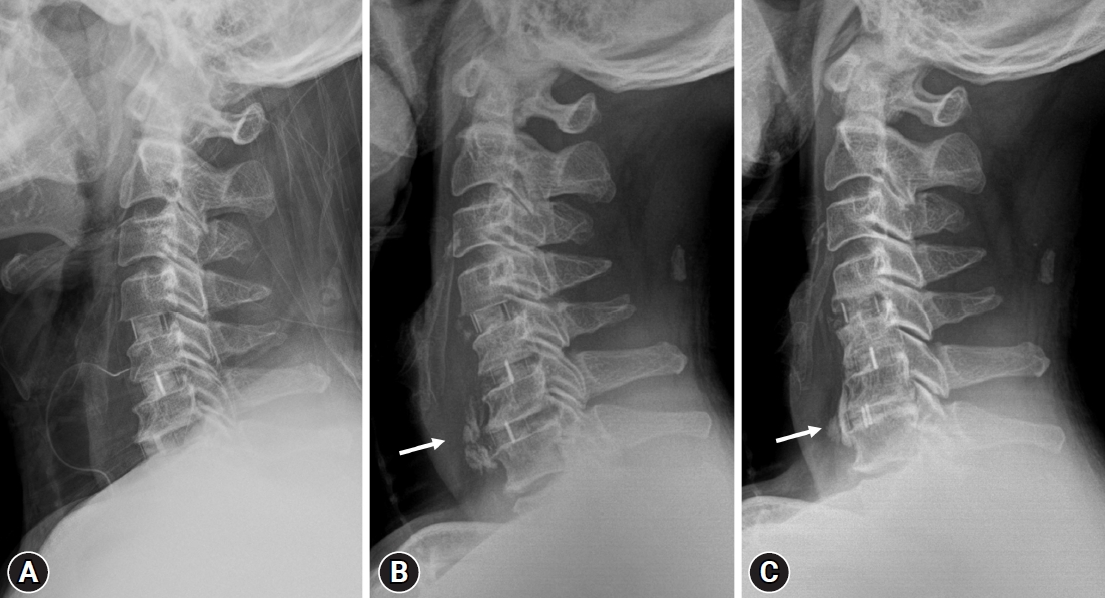
A 60-year-old male patient was admitted to our hospital with right arm motor weakness, severe posterior neck pain, and right arm radiating pain. Physical examination revealed right shoulder elevation grade III, right elbow flexion grade IV, wrist extension grade V, elbow extension grade V, and hand grasp grade V. Moderate hypesthesia was observed in the C7, 8 sensory dermatomes. Magnetic resonance imaging (MRI) revealed herniated discs at the C4–5, C5–6, and C6–7 levels, compressing the right side of the nerve root. Based on physical examination and radiologic findings, we decided to perform stand-alone ACDF surgery at the C4–5–6–7 level. Under general anesthesia, a Standard Smith-Robinson method was used to expose the involved segment. After discectomy, the upper and lower cartilaginous endplates were decorticated, preserving the bony endplates. Local autologous bone chips were collected during removal of osteophytes for grafting. The appropriate PEEK cage was selected (Solis cage; Stryker, Allendale, NJ, USA/Cornerstone cage; Medtronic, Memphis, TN, USA), filled with an i-factor 2.5 mL divided into 1/3 that was intermixed with autologous bone chips, and inserted into the disc space (Fig. 1A). After surgery, the patient’s motor weakness, posterior neck pain, and radiating pain improved, and he was discharged without any complications. However, the patient developed mild dysphagia 1 month after surgery. A simple cervical spine radiograph showed unexpected bone formation in the anterior portion of the vertebral body at C6 and C7 levels (Fig. 1B). Since the patient’s dysphagia was not severe, after careful consideration, we decided to administer conservative treatment and follow-up without removing the unexpectedly formed bone through revision surgery. The patient’s dysphagia gradually improved, and the symptoms of dysphagia disappeared 1 year after surgery. In addition, simple cervical radiograph 1 year after surgery revealed that a part of the unexpected bone formed in the anterior portion of the vertebral body remained, although some was absorbed (Fig. 1C).
2. Case 2
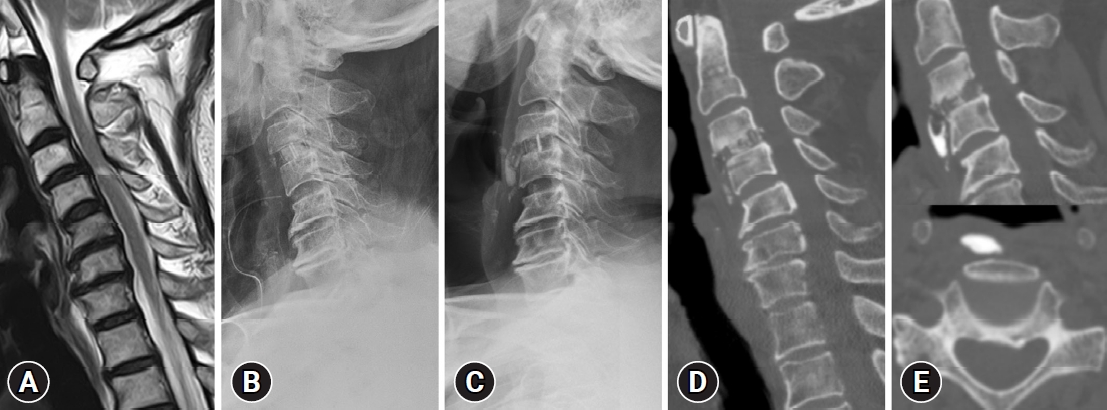
A 67-year-old male patient was admitted to our hospital with right arm motor weakness and right arm radiating pain that had begun 1 week prior. Physical examination showed right shoulder elevation grade I, right elbow flexion grade III, wrist extension grade V, elbow extension grade V, and hand grasp grade V. Moderate hypesthesia was observed in the C5 sensory dermatomes. MRI revealed a herniated disc at the C3–4 level, compressing the spinal cord and causing myelopathy (Fig. 2A). Based on physical examination and radiologic findings, we decided to perform stand-alone ACDF surgery at the C3–4 level. Under general anesthesia, a Standard Smith-Robinson method was used to expose the involved segment. After discectomy, the upper and lower cartilaginous endplates were decorticated, preserving the bony endplates. Local autologous bone chips were collected during removal of osteophytes for grafting. The appropriate PEEK cage was selected (Solis cage; Stryker, Allendale, NJ, USA), filled with 1 mL of i-factor 1 mL that was intermixed with autologous bone chips, and inserted into the disc space (Fig. 2B). After surgery, the patient’s motor weakness and radiating pain improved, and the patient was discharged without any complications. However, the patient developed mild dysphagia 3 months after surgery. A simple cervical spine radiograph showed unexpected bone formation in the anterior portion of the vertebral body at the C3 and 4 levels (Fig. 2C). Computed tomography (CT) scan revealed the presence of a bridging bone at the graft level, but showed unexpected bone formation in the anterior portion of the vertebral body (Fig. 2D, E). We recommended revision surgery to remove the unexpectedly formed bone. However, the patient did not wich to undergo additional surgery as the dysphagia was mild and symptoms related to the right arm had improved. The unexpected bone formation was not absorbed and remained unchanged on follow-up simple cervical spine radiograph 1 year after surgery, but the patient’s dysphagia gradually improved.
DISCUSSION
Fusion rates in spine surgery are steadily increasing and accelerating with the development of various bone-inductive substances, including demineralized bone matrix, recombinant human bone morphogenetic proteins, and i-factor. i-Factor is a combination product consisting of P-15 adsorbed onto anorganic bone mineral and suspended in an insert biocompatible hydrogel carrier. P-15 is a novel synthetic 15-amino-acid polypeptide that mimics the cell-binding domain of type I collagen [13,14]. The P-15 peptide promotes cell migration and induces osteoblast cell proliferation and differentiation. P-15 appears to promote the differentiation of human bone marrow stromal cells into osteoblasts and induce production and secretion of osteogenic factors that drive other cells to adopt an osteoblastic phenotype [15]. This can signal a mechanical and biochemical communication pathway resulting in new bone formation [15,16]. This product has demonstrated safety and efficacy as a bone graft substitute for this application, and has subsequently gained US Food and Drug Administration (FDA) approval for single-level ACDF from C3 to C7 [12].
Because of their potent bone-inductive capacities, several theoretical safety issues arise when considering the use of the i-factor in spinal fusion. These issues include the potential for carcinogenicity, systemic toxicity, immune responses, and uncontrolled bone formation of adjacent discs and soft tissues leading to neural structure compression. However, despite these theoretical concerns, clinical studies with i-factor have thus far been very favorable and failed to demonstrate any such adverse events related to i-factor when it is inserted through an anterior approach for cervical interbody fusion [11,12]. Arnold et al. [11,12] revealed that among patients who underwent ACDF, the patient group using i-factor had a fusion rate of 88.97% in the 1st year and 97.30% in the 2nd year, which were higher than those in the group using autograft. Although they did not reveal the fusion achieved interval and exact i-factor usage capacity for each level where ACDF was performed, the average i-factor usage capacity was 0.78 mL (range 0.15–4.0 mL). Regarding adverse events, dysphagia occurred in 19.25% cases of the group using the i-factor and in 19.74% cases of the ACDF group using the autograft. However, they could not identify the relationship with the i-factor.
We observed unexpected bone formation causing dysphagia after ACDF using the i-factor in two cases. In the first case, 0.83 mL i-factor was used per level, and in the second case, 1 mL i-factor was used per level. There are several possible explanations for the unexpected bone formation in the anterior portion of the vertebral body. First, since there is no precise dose guideline per level or inside the cage, and because i-factor is expensive and helps achieve fusion, clinicians try to use as many i-factors as possible (Fig. 3A). Second, some i-factor leaks out while inserting the cage into the disc space with the maximum amount of i-factor in the cage (Fig. 3B). In addition, if water irrigation is performed in this state, not only the leaked i-factor, but also the i-factor inside the cage may be lost; thus clinicians should refrain from using water irrigation. Consequently, the leaked i-factor is deposited in a specific area, causing unexpected bone formation.
Further biomechanical studies are needed to determine the optimal dose of i-factor to help in fusion while preventing excessive bone formation. Until this is determined, we suggest that clinician should use i-factor appropriately. When filling the cage with the i-factor intermixed with autogenous bone chips, clinicians should be careful to ensure that the cage is filled without any overflow. Although wasteful, the remaining i-factor should be discarded. Even if clinicians should avoid water irrigation after cage insertion, clinicians should remove any i-factor leaking out of the cage or into the disc space using forceps or cottonoid with a cleanser (Fig. 3C). Moreover, hasty revision surgery is not recommended in cases of unexpected bone formation after surgery, as it can be absorbed over time, and the patient’s symptoms may improve.
In conclusion, we report two cases of adverse events after ACDF using i-factor. The unexpected bone formation causing dysphagia that we observed may be due to the high potent bone-inductive capacity of i-factor, but instead because there are no guidelines on proper dosage and usage. Further biomechanical studies are required to determine the optimal dose and usage instruction of i-factor, and clinicians should use i-factor appropriately in the meantime.